Screenshots
|
Benefits
|

|
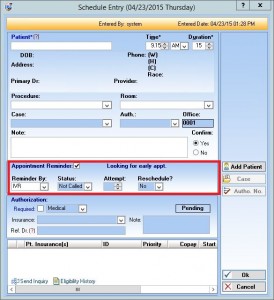
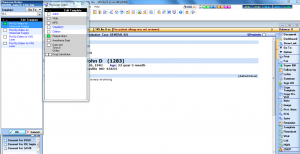
Patient Appointment Scheduling
With an intuitive, customizable appointment scheduler, doctors and staff can easily manage patient appointments – including schedules for multiple offices and providers.
* Click Screenshot To Expand |
- Reduce missed appointments
- Improve office productivity
- Eliminate overbookings
|

|
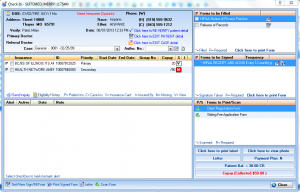
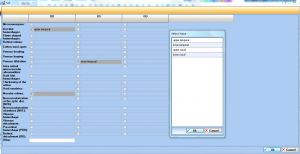
Eligibility Tracking
Determine the status of your patients' insurance coverage prior to the date of service with IMS' eligibility verification module.
* Click Screenshot To Expand |
- Reduce rejected claims
- Save staff time
- Increase revenue
- Improve patient relationships
|
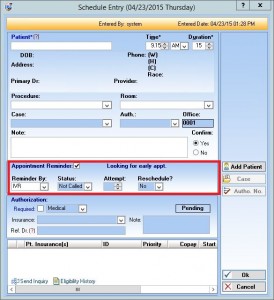 |
Patient Reminders
IMS' Interactive Voice Reminders service integrates with the appointment scheduling software to ensure that all of your patients receive reminders about their upcoming appointments.
* Click Screenshot To Expand |
- Use live-person and automated reminders
- Decrease missed appointments
- Increase productivity
- Improve patient satisfaction
|
 |
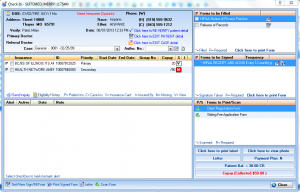
Check-In/Check-Out
IMS' check-in/check-out feature allows staff to manage patients as they move about the office during their visit. This starts with the initial intake and ends at check out.
* Click Screenshot To Expand |
- Keep track of patients
- Improve intra-office communication
- Effectively manage office resources
|
|
CHECK-IN
Achieve a truly paperless environment with IMS' patient check-in module. It covers all aspects of the intake process from updating patient data to collecting co-pays or co-insurances.
* Click Screenshot To Expand |
- Achieve maximum efficiency
- Streamline workflow
- Reduce check-in time
|
|
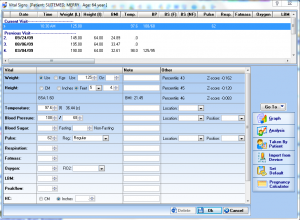
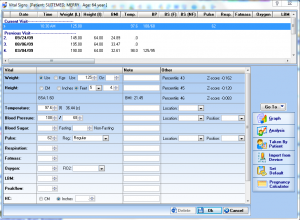
Vitals Interface
With IMS, patient vitals can be transferred wirelessly from your vitals device to the EHR. Vitals auto-populate in the patient's chart, eliminating data entry and reducing errors.
* Click Screenshot To Expand |
- Facilitates efficient data transfer
- Meets HIPAA standards
- Compliant with HL7, CCD, CCR
|
   |
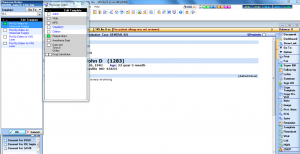
Patient health record
Document patient visits quickly and easily with IMS' specialty-specific templates. Use our intuitive visit notes, customize them to meet your unique charting needs, or create your own.
* Click Screenshot To Expand |
- Increase efficiency
- Improve documentation
- Enhance patient care
|
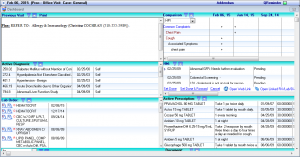 |
Patient Dashboard
IMS' Patient Dashboard offers a summary of all patient information stored within the EHR. Here, providers can view data such as demographics, problems, medications, and more.
* Click Screenshot To Expand |
- Get important information at-a-glance
- Better understand your patients' health
- Make more informed decisions
|

|
Dictation
With IMS' seamless speech recognition feature, providers can dictate notes in screens throughout the EHR and receive them immediately for review.
* Click Screenshot To Expand |
- Improve the completeness of notes
- Save on transcription costs
- Improve productivity
- Simplify workflow
|

|
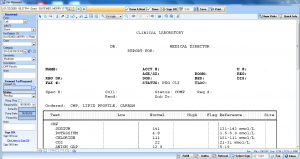
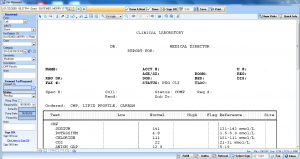
Lab & Diagnostic orders
Submit lab orders and diagnostic tests electronically and track results directly through your EHR. Receive a notification as soon as results are received and quickly file them in the patient's chart.
* Click Screenshot To Expand |
- Track patient care more efficiently
- Make better use of office resources
- Meet Meaningful Use requirements
- Streamline workflow
|
|
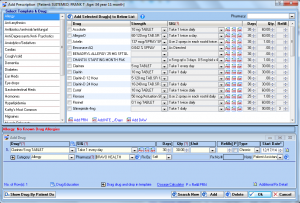
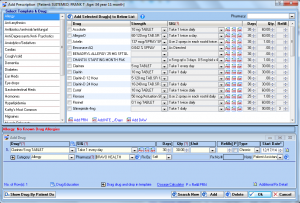
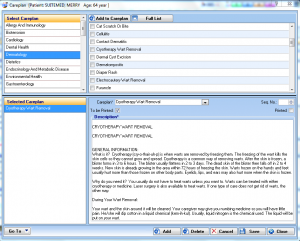
E-prescribing
Manage patient medications with IMS' e-prescribing module. Our EHR features fax and electronic prescription submission, medication tracking, dosing information, and more.
* Click Screenshot To Expand |
- Streamline prescription management
- Reduce data entry errors
- Increase patient safety
- Meet Meaningful Use requirements
|
|
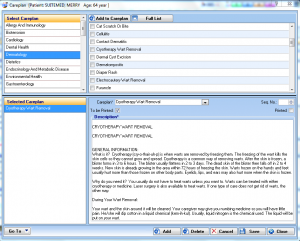
Care Plans
Come up with a care plan for your patients, and IMS EHR will generate a patient education handout based on the selected diagnosis and condition.
* Click Screenshot To Expand |
- Increase patient engagement
- Improve quality of care
|
 |
Check-Out
Ensure that all pending items are resolved before patients leave your office. Our check-out feature will prompt you to schedule follow-up appointments, collect the patient responsibility, and more.
* Click Screenshot To Expand |
- Increase collections
- Make better use of staff resources
- Improve patient satisfaction
|
|
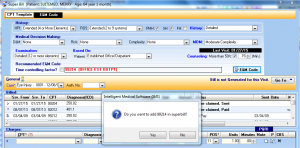
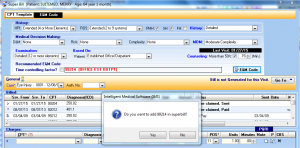
e&m coder
IMS' CPT Coding Advisor will review factors such as HPI and time spent with the patient and recommend appropriate E&M codes to ensure that payer documentation needs are adequately met.
* Click Screenshot To Expand |
- Pre-screen claims automatically
- Check authorization requirements
- Reduce denials
|
|
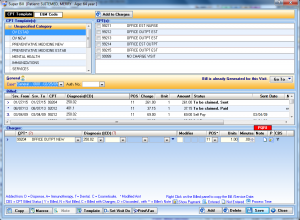
Electronic Super Bill
Create electronic super bills directly from your EHR for quick and simplified charge entry. You can even customize the super bills to meet the needs of each provider in your practice.
* Click Screenshot To Expand |
- Capture all charges from your patient visits
- Reduce paper expenses
- Eliminate lost or missing forms
|
 |
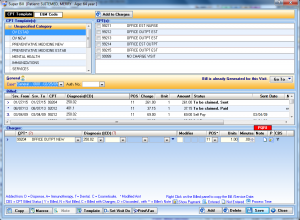
Receivables tracking
Streamline office functions, see fewer missed payments, and help your practice run more efficiently than ever with IMS' Revenue Cycle Management software.
* Click Screenshot To Expand |
- Automate data entry
- Maximize revenue
- Increase productivity
|
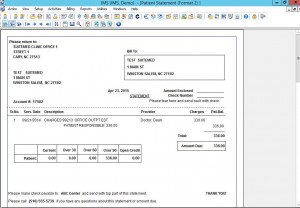 |
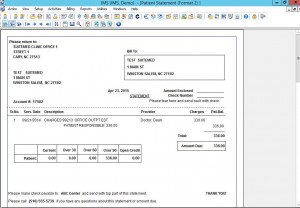
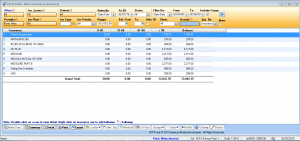
billflash Patient Statements
Transmit patient statements electronically and resolve collection issues more efficiently with our automated statement processing service.
* Click Screenshot To Expand |
- Increase efficiency
- Reduce accounts receivable
- Eliminate forms and paper-based costs
|

|
electronic Patient Payments
Our EHR-integrated patient payment solution allows providers to securely collect payments from patients in person, online, and over the phone.
* Click Screenshot To Expand |
- Provide multiple payment options
- Increase revenue
- Improve patient satisfaction
|
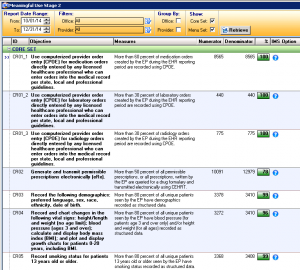 |
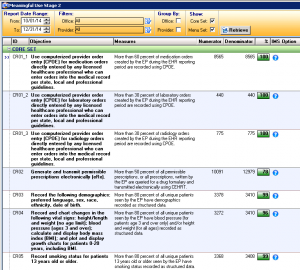
Meaningful Use Dashboard
Manage and track your Meaningful Use progress with our interactive Meaningful Use Reporting module. Gather real-time indicators of current Meaningful Use levels, view percentages of compliancy, and more.
* Click Screenshot To Expand |
- Ensure attestation objectives are met
- Meet Meaningful Use requirements
- Monitor problem areas daily
|
 |
Task List
IMS' Personal My Tasks List alerts doctors and staff about unfinished tasks that can affect patient care. This includes notifications regarding lab results, unsigned visit notes, and more.
* Click Screenshot To Expand |
- Track patient care from start to finish
- Improve intra-office communication
- Achieve maximum productivity
- Improve office workflow
|
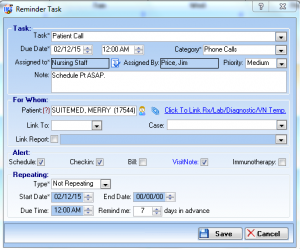 |
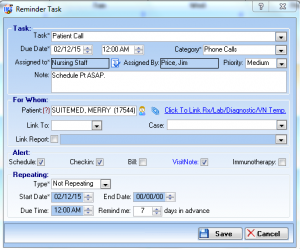
Tasks and Reminders
Fully integrated modules within IMS alert doctors and staff of important tasks related to patient care. This includes follow-up appointments, specialist referrals, medication management, and many more.
* Click Screenshot To Expand |
- Improve preventive care efforts
- Increase practice productivity
- Provide better patient care
- Customize alerts to your specialty
|
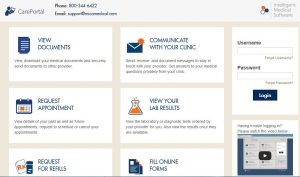 |
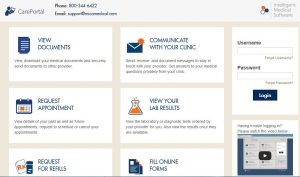
Patient Portal
Involve patients in their health care by offering access to an online patient portal. With our portal, your patients will be able to view visit summaries and test results, request medication refills, and much more.
* Click Screenshot To Expand |
- Streamline administrative processes
- Reduce workload
- Increase patient satisfaction
- Meet Meaningful Use requirements
|
 |
Patient Special Search
This powerful feature allows providers to query their patient population for particular reasons, by searching on any box or field within the EHR.
* Click Screenshot To Expand |
- Send correspondence to multiple patients
- Generate lists by specific condition
- Export queried lists for future reference
|
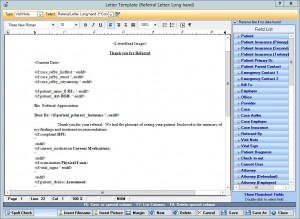 |
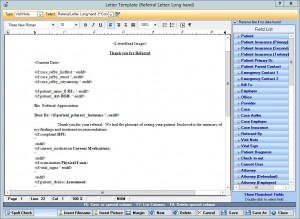
Letters/Forms Automation
IMS EHR features specialty-specific forms and letters that providers in your field use most. You also have the option of generating custom documents with the input fields of your choice.
* Click Screenshot To Expand |
- Eliminate paper forms
- Save time
- Improve productivity
|
 |
Authorization Tracking
IMS' powerful Authorization Tracking module will help your practice track and manage all patient authorizations from one place in your EHR.
* Click Screenshot To Expand |
- Pre-validate procedures quickly and easily
- Make better use of staff resources
- Improve productivity
|
 |
cloud based faxing
With IMS' integrated fax module, providers can send faxed documents directly into patients' charts without scanning and fax patient data from the EHR.
* Click Screenshot To Expand |
- Reduce paper and printing costs
- Improve productivity
- Maximize efficiencies
- Enhance workflows
|
 |
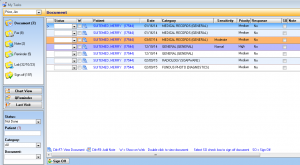
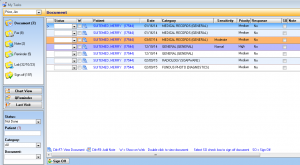
Document management
Create a custom list of folders and subfolders to manage documents stored in each of your patients' charts. Documents can then be faxed or emailed directly from the EHR.
* Click Screenshot To Expand |
- Organize documents more efficiently
- Easily find pertinent information
- Increase productivity
|
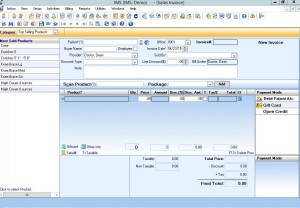 |
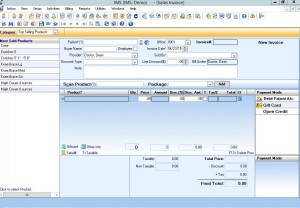
Point of Sale/inventory management
From bar code scanning to inventory management, IMS' point of sale capabilities will allow you to run a more efficient practice by ensuring you have the right supplies on hand at all times.
* Click Screenshot To Expand |
- Streamline the check-out process
- Increase profits
- Maximize efficiency
|
 |
referral Marketing management
Help make marketing decisions, keep track of marketing expenses, and take advantage of custom reporting capabilities with our EHR-integrated marketing module.
* Click Screenshot To Expand |
- Manage and organize leads
- Increase revenue
- Improve patient recall and retention
|
 |
Health Maintenance Tracking
Keep track of patients' health with IMS' health maintenance tracking feature. Physicians receive alerts when things are due, when patients need a follow-up call, when lab results are in, and more.
* Click Screenshot To Expand |
- Improve patient health
- Provide better care quality
- Increase patient satisfaction
- Improve practice efficiencies
|
 |
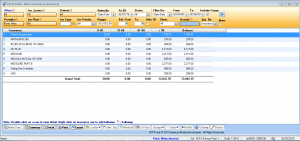
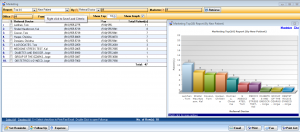
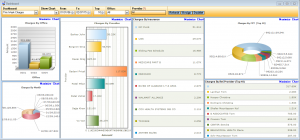
graphical analytics
Find out how your practice is doing by running billing reports and graphs with a click of a button. Graphs can be generated by provider, insurance carrier, procedure, referring provider, and more.
* Click Screenshot To Expand |
- Monitor your practice's finances
- Increase collections
|
 |
Referral Tracking
With IMS' referral tracking module, providers can track incoming and outgoing referrals, manage referral sources, and market to referring providers in their area.
* Click Screenshot To Expand |
- Streamline communication
- Build relationships with other providers
- Improve productivity
|
 |
Reports Center
Create a variety of reports – everything from billing to Meaningful Use – to help manage your pain management practice as efficiently as possible.
* Click Screenshot To Expand
|
- Meet Meaningful Use Requirements
- Monitor practice goals
- Maximize efficiencies
- Make better use of staff resources
|